- Vol 66 No 6
- Volume 66
- Issue 06
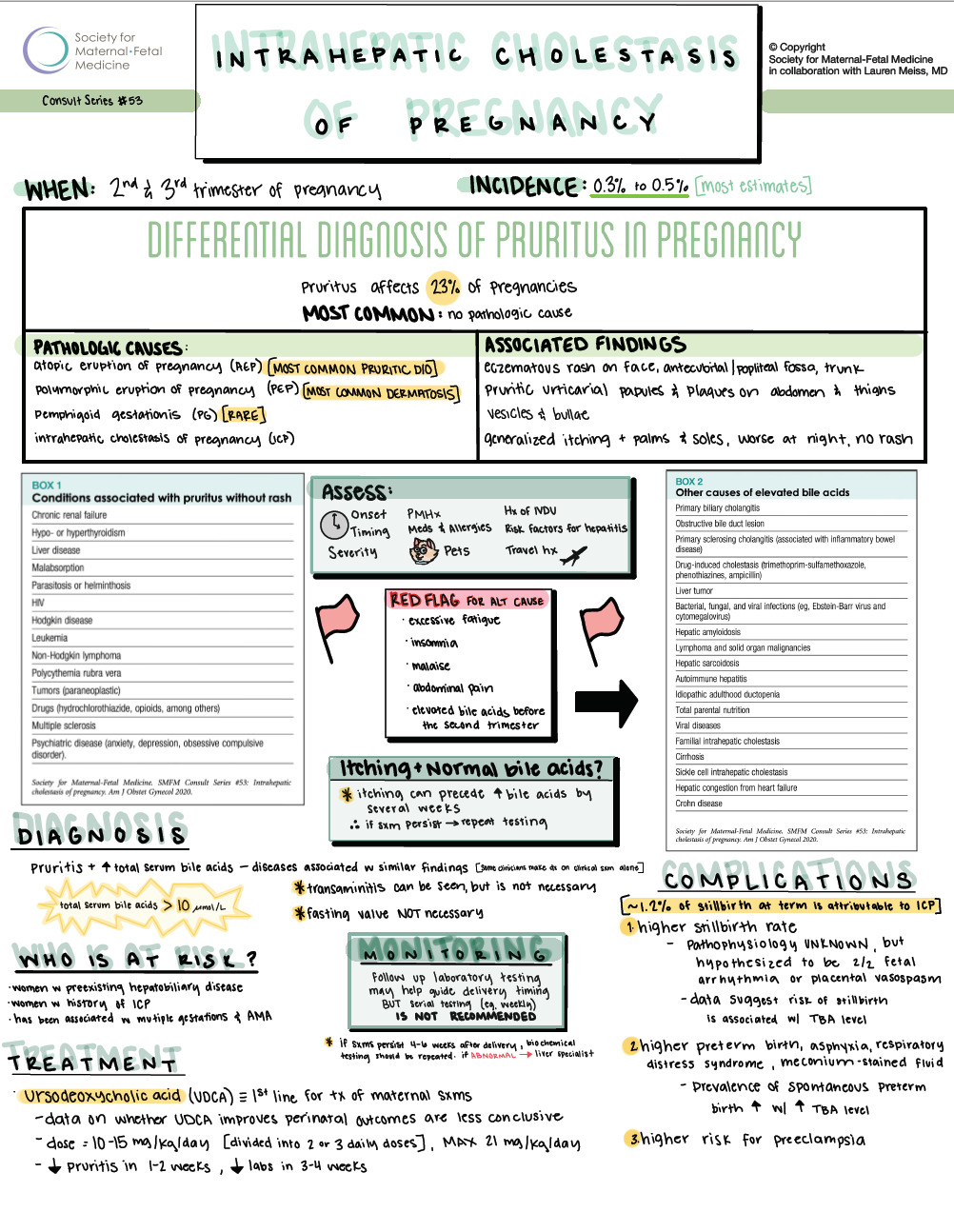
Society for Maternal-Fetal Medicine Consult Series #53: Intrahepatic Cholestasis of Pregnancy

Intrahepatic cholestasis of pregnancy (ICP) occurs in the second and third trimesters of pregnancy and is characterized by pruritus and elevated serum bile acid concentrations.
Intrahepatic cholestasis of pregnancy (ICP) occurs in the second and third trimesters of pregnancy and is characterized by pruritus and elevated serum bile acid concentrations. Its incidence has been estimated to range from 0.3% to 15% in various populations, with most estimates from 0.3% to 0.5%.1 While ICP poses little risk for women, it does confer risk to the fetus. The persistence and intensity of associated pruritis are uncomfortable, and the increased risk of stillbirth is a significant concern to both patients and health care professionals.
Q|What is the differential diagnosis of pruritis in pregnancy?
Pruritis is a common complaint in pregnancy.2 In ICP, itching is often generalized but predominantly affects the palms of the hands and the soles of the feet, is worse at night, and is generally not associated with a rash.2 The most frequent pathologic causes of pruritus specific to pregnancy include atopic eruption of pregnancy, polymorphic eruption of pregnancy, pemphigoid gestationis, and ICP.3
Q|How should a woman with pruritus in pregnancy be evaluated?
A detailed history and physical examination are imperative in making the diagnosis of ICP. In the process of taking the history and performing the physical examination, it is appropriate to consider and assess for other causes of pruritus without a rash (Box 1). ICP should be considered in a woman who develops new-onset pruritus without a rash in the second half of pregnancy.
In evaluating a patient for other potential causes for pruritus, one should assess the onset, extent, severity, aggravating and alleviating factors, timing, medical history, medications (eg, narcotics), allergies, past medical/family history of atopy (eg, eczema, allergic rhinitis, asthma), amount of bathing, household contacts, pets, and travel history. Sexual history and any history of intravenous drug use should be assessed to ascertain the patient’s risk of hepatitis and HIV. A history of ICP in any prior pregnancies should be assessed as well.
Other significant signs and symptoms to assess include recent changes in weight, appetite, skin or eye color (jaundice), and sleep habits. Excessive fatigue, insomnia, malaise, and abdominal pain and colic are not common with ICP. If present, evaluation for other causes of pruritis and hepatic disease may be warranted.
The physical examination should assess for the presence of rashes, excoriations, papules, plaques, or bullae. Although ICP is not associated with a rash, the intensity of the pruritus can lead to the development of excoriations or prurigo nodularis, which may be mistaken for a rash.4 Dark urine and jaundice are not common with ICP and suggest other hepatic diseases.
Q|What laboratory evaluation is recommended for a pregnant woman with pruritis in whom ICP is suspected?
We recommend measurement of serum bile acid levels and liver transaminases in patients with suspected ICP (GRADE 1B). Mass spectrometry and liquid chromatography can evaluate for total and fractionated (cholic, chenodeoxycholic, and deoxycholic acid) bile acids. Total bile acids also can be assessed by enzymatic assay. Although the enzymatic assay does not provide fractionated bile acid levels, fractionated levels have limited utility, and the most clinically useful value is the total bile acid level.
The clinical diagnosis of ICP is based on pruritus symptoms and supported by the presence of elevated total serum bile acid levels and the absence of diseases associated with similar laboratory findings and symptoms. A serum total bile acid concentration of greater than 10 micromol/L often is used to diagnose ICP, although the data are limited and the diagnostic accuracy has been questioned.5,6 Increases in transaminases (eg, alanine aminotransferase and aspartate aminotransferase) can also sometimes be seen in ICP, although elevated transaminases are not necessary for the diagnosis.
Although bile acid levels can be affected by a postprandial state, random bile acids can be used to diagnose ICP and are typically more convenient for the patient and practitioner than fasting bile acids. Box 2 lists other causes of ICP and elevated bile acid concentrations. Particularly in women with elevated bile acids before the second trimester of pregnancy, other etiologies should be considered.
Q|Are particular women or populations at risk for ICP?
Women with preexisting hepatobiliary disease are reported to be at higher risk for ICP. Patients with a history of ICP are at risk for recurrence. ICP has been associated with multiple gestations and advanced maternal age, and familial clustering of cases of ICP also suggests a genetic component.7 ICP likely results from both environmental and hormonal influences in women who are genetically susceptible.
Q|What are the complications of cholestasis of pregnancy?
ICP is associated with several adverse perinatal outcomes, including stillbirth, meconium-stained amniotic fluid, and preterm birth (both spontaneous and iatrogenic). Data suggest that the risk of stillbirth with ICP is associated with the total bile acid concentration,8,9 although some level of risk may still be present even with low bile acid concentrations.
Women with ICP and bile acid levels ≥40 micromol/L have been reported to have increased risks of adverse perinatal outcomes, including preterm birth, asphyxia or respiratory distress syndrome, and meconium-stained amniotic fluid.10 Increased rates of both indicated and spontaneous preterm birth are reported with ICP, with the incidence of prematurity varying greatly among studies. Pregnancies complicated by spontaneous preterm birth have been reported to have an earlier onset of pruritus, and the prevalence of spontaneous preterm birth increases with higher total bile acid concentrations.11,12 There also is evidence that patients with ICP are at increased risk for preeclampsia.1
Q|What is the recommended treatment for cholestasis of pregnancy?
We recommend that ursodeoxycholic acid (UDCA) be used as the first-line agent for the treatment of maternal symptoms of ICP (GRADE 1A). Three meta-analyses have summarized the data from randomized trials and have reported benefits in improving maternal symptoms.13-15 Compared with placebo or alternative agents (eg, cholestyramine or S-adenosyl methionine), UDCA is more effective in relieving pruritus and improving laboratory abnormalities and has no known adverse fetal effects. The typical starting dose for UDCA is 10 to 15 mg/kg per day, which can be divided into doses taken 2 or 3 times daily. Typical regimens are 300 mg taken 2 or 3 times daily or 500 mg twice daily. A decrease in pruritus usually is seen within 1 to 2 weeks. If pruritis is not relieved, the dose can be titrated to a maximum of 21 mg/kg per day. Biochemical improvement is usually seen within 3 to 4 weeks.
Alternative drugs, such as S-adenosyl methionine and cholestyramine, can be considered for patients who cannot take UDCA or have continued symptoms on the maximum dosage. It has been reported that rifampin can be combined with UDCA for refractory cases of ICP with improvement in pruritis.16 Antihistamines such as diphenhydramine or hydroxyzine also have been used for pruritis, although these may have limited benefit. Topical antipruritics (eg, menthol creams, calamine lotion) are also of limited use, given that itching is typically widespread. To date, none of these alternative treatments have been evaluated in randomized controlled trials.
Q|Is serial serum bile acid testing beneficial?
In patients with ICP, bile acid levels can increase during pregnancy and may increase rapidly near term. Given that higher serum total bile acid concentrations have been associated with adverse perinatal outcomes in some studies, repeat bile acid measurement has been suggested as potentially useful in guiding management. Follow-up laboratory testing may help guide delivery timing, especially in severe cases, but serial testing (eg, weekly) is not recommended.
Q|How should a pregnant woman with itching and normal bile acids be managed?
The pruritus in ICP can precede the rise in serum bile acids by several weeks. Therefore, if symptoms persist and no other explanation for pruritis exists, measurement of the total bile acid concentration and serum transaminases should be repeated. If UDCA is started empirically at the time testing is performed and before results are available, it is possible that elevated bile acid or transaminase levels may never be detected.
Q|Is antepartum testing indicated for patients with ICP?
We suggest that patients with a diagnosis of ICP begin antenatal fetal surveillance at a gestational age when delivery would be performed in response to abnormal fetal testing or at the time of diagnosis if the diagnosis is made later in gestation (GRADE 2C). The observed increased risk of stillbirth with ICP has prompted most practitioners to perform antenatal testing in this setting. However, the efficacy of antepartum fetal testing to prevent stillbirth in the setting of ICP is unknown. Several studies and case reports have reported stillbirth occurring within a few days of a reactive nonstress test.17-20 Antepartum fetal testing in ICP may not be useful because the mechanism of stillbirth is thought to be a sudden event rather than a chronic placental vascular process.
Recent clinical trials and meta-analyses support fetal surveillance with substantially lower rates of adverse perinatal outcomes compared with earlier reports, potentially due to more intensive monitoring with fetal surveillance and late-preterm or early-term delivery.11,14,21 The optimal frequency of testing is unknown and may be determined by criteria such as comorbidities or bile acid levels (eg, more frequent for total bile acid levels of 100 micromol/L or more). Due to the higher risk of stillbirth, patients with ICP should be placed on continuous fetal monitoring in labor.
Q| When should women with a diagnosis of cholestasis be delivered?
While the risk for late stillbirth is avoided with an early planned delivery, this must be weighed against risks to the neonate related to prematurity. The timing of delivery should be approached using risk stratification based on patient-specific factors, including total bile acid levels, in a shared decision-making model. We recommend that patients with total bile acid levels ≥100 micromol/L be offered delivery at 36 0/7 weeks of gestation, given that the risk for stillbirth increases substantially around this gestational age (GRADE 1B). We recommend delivery between 36 0/7 and 39 0/7 weeks of gestation for patients with intrahepatic cholestasis of pregnancy and total bile acid levels <100 micromol/L (GRADE 1C). Delivery timing for women with total bile acid levels <100 micromol/L should be individualized; it is reasonable for patients with bile acid levels of <40 micromol/L to be managed toward the later end of this time range, given the low risk for stillbirth seen in the studies referenced above, while women with total bile acid levels of ≥40 micromol/L should be considered for earlier delivery.
Delivery between 34 and 36 weeks of gestation can be considered in women with ICP, total bile acid levels of ≥100 micromol/L, and any of the following:
- excruciating and unremitting maternal pruritus not relieved with pharmacotherapy;
- a prior history of stillbirth before 36 weeks of gestation due to ICP with recurring ICP in the current pregnancy; or
- preexisting or acute hepatic disease with clinical or laboratory evidence of worsening hepatic function.
Any patient delivered for ICP prior to 36 weeks of gestation should be extensively counseled about the absence of definitive evidence that the maternal and fetal benefits of delivery outweigh the potential morbidity of prematurity. We recommend antenatal corticosteroids for fetal lung maturity for patients delivered before 37 0/7 weeks of gestation if not previously treated (GRADE 1A).
For patients with early-term pregnancies (37 to 38 weeks of gestation) with pruritis suggestive of ICP, no rash, and no bile acid results yet available to confirm the diagnosis, management should be based on shared decision-making that involves a discussion of the uncertainty of the diagnosis, the risks of ICP vs early-term delivery, and the values and preferences of the patient.
Diagnostic certainty, and thus advice about delivery management, is improved if there are elevated transaminases or a history of ICP in prior pregnancies, and it may be reasonable to deliver in the absence of bile acid results in these situations. We recommend against preterm delivery at <37 weeks of gestation in patients with a clinical diagnosis of ICP without laboratory confirmation of elevated bile acids (GRADE 1B).
Q|What is the likelihood of recurrence?
The risk of recurrence of ICP in subsequent pregnancies may be as high as 90%, although data are insufficient to counsel patients on specific ranges.12 Some data also suggest that patients with a history of ICP are at higher risk for developing later hepatobiliary disease, particularly within the first year after the diagnosis of ICP. Given the risk for hepatitis C in these patients and the availability of an effective treatment, some experts advocate for routine testing for hepatitis C in patients with ICP.22
It is important to consider reevaluation of liver function test results after delivery in patients with persistent pruritis or other signs or symptoms of a hepatobiliary disease, such as right upper quadrant pain or jaundice. If serologic study results remain abnormal, the patient should be referred to a liver specialist for evaluation for another underlying condition.
References
1.Wikström Shemer E, Marschall HU, Ludvigsson JF, Stephansson O. Intrahepatic cholestasis of pregnancy and associated adverse pregnancy and fetal outcomes: a 12-year population-based cohort study. BJOG 2013;120:717-23.
2.Kenyon AP, Tribe RM, Nelson-Piercy C, et al. Pruritus in pregnancy: a study of anatomical distribution and prevalence in relation to the development of obstetric cholestasis. Obstet Med 2010;3:25-9.
3.Bechtel MA, Plotner A. Dermatoses of pregnancy. Clin Obstet Gynecol 2015;58:104-11.
4.Ambros-Rudolph CM, Glatz M, Trauner M, Kerl H, Müllegger RR. The importance of serum bile acid level analysis and treatment with ursodeoxycholic acid in intrahepatic cholestasis of pregnancy: A case series from central europe. Arch Dermatol 2007;143:757-62.
5.Egan N, Bartels A, Khashan AS, et al. Reference standard for serum bile acids in pregnancy. BJOG : 2012;119:493-8.
6.Manzotti C, Casazza G, Stimac T, Nikolova D, Gluud C. Total serum bile acids or serum bile acid profile, or both, for the diagnosis of intrahepatic cholestasis of pregnancy. Cochrane Database Syst Rev 2019;7:Cd012546.
7.Pataia V, Dixon PH, Williamson C. Pregnancy and bile acid disorders. Am J Physiol Gastrointest Liver Physiol 2017;313:G1-g6.
8.Brouwers L, Koster MP, Page-Christiaens GC, et al. Intrahepatic cholestasis of pregnancy: maternal and fetal outcomes associated with elevated bile acid levels. Am J Obstet Gynecol 2015;212:100 e1-7.
9.Kawakita T, Parikh LI, Ramsey PS, et al. Predictors of adverse neonatal outcomes in intrahepatic cholestasis of pregnancy. Am J Obstet Gynecol 2015;213:570 e1-8.
10.Cui D, Zhong Y, Zhang L, Du H. Bile acid levels and risk of adverse perinatal outcomes in intrahepatic cholestasis of pregnancy: A meta-analysis. J Obstet Gynaecol Res 2017;43:1411-20.
11.Ovadia C, Seed PT, Sklavounos A, et al. Association of adverse perinatal outcomes of intrahepatic cholestasis of pregnancy with biochemical markers: results of aggregate and individual patient data meta-analyses. Lancet 2019;393:899-909.
12.Williamson C, Hems LM, Goulis DG, et al. Clinical outcome in a series of cases of obstetric cholestasis identified via a patient support group. BJOG 2004;111:676-81.
13.Bacq Y, Sentilhes L, Reyes HB, et al. Efficacy of ursodeoxycholic acid in treating intrahepatic cholestasis of pregnancy: a meta-analysis. Gastroenterology 2012;143:1492-501.
14.Gurung V, Middleton P, Milan SJ, Hague W, Thornton JG. Interventions for treating cholestasis in pregnancy. Cochrane Database Syst Rev 2013;2013:Cd000493.
15.Kong X, Kong Y, Zhang F, Wang T, Yan J. Evaluating the effectiveness and safety of ursodeoxycholic acid in treatment of intrahepatic cholestasis of pregnancy: A meta-analysis (a prisma-compliant study). Medicine (Baltimore) 2016;95:e4949.
16.Liu J, Murray AM, Mankus EB, Ireland KE, Acosta OM, Ramsey PS. Adjuvant Use of Rifampin for Refractory Intrahepatic Cholestasis of Pregnancy. Obstet Gynecol 2018;132:678-81.
17.Alsulyman OM, Ouzounian JG, Ames-Castro M, Goodwin TM. Intrahepatic cholestasis of pregnancy: perinatal outcome associated with expectant management. Am J Obstet Gynecol 1996;175:957-60.
18.Herrera CA, Manuck TA, Stoddard GJ, et al. Perinatal outcomes associated with intrahepatic cholestasis of pregnancy. The Journal of Maternal-Fetal & Neonatal Medicine 2018;31:1913-20.
19.Lee RH, Incerpi MH, Miller DA, Pathak B, Goodwin TM. Sudden fetal death in intrahepatic cholestasis of pregnancy. Obstet Gynecol 2009;113:528-31.
20.Sentilhes L, Verspyck E, Pia P, Marpeau L. Fetal death in a patient with intrahepatic cholestasis of pregnancy. Obstet Gynecol 2006;107:458-60.
21.Chappell LC, Bell JL, Smith A, et al. Ursodeoxycholic acid versus placebo in women with intrahepatic cholestasis of pregnancy (PITCHES): a randomised controlled trial. Lancet 2019;394:849-60.
22.Wijarnpreecha K, Thongprayoon C, Sanguankeo A, Upala S, Ungprasert P, Cheungpasitporn W. Hepatitis C infection and intrahepatic cholestasis of pregnancy: A systematic review and meta-analysis. Clin Res Hepatol Gastroenterol 2017;41:39-45.
Articles in this issue
over 4 years ago
Beyond the Pandemic: Articles and Resources for Self-Educationover 4 years ago
ACOG 2021: Beyond the Pandemicover 4 years ago
Acute Fatty Liver of Pregnancyover 4 years ago
New Mother's Thumbover 4 years ago
What's New in Women's Health?over 4 years ago
Moving Beyond Checking the Boxover 4 years ago
US Women’s Sexual and Reproductive Health Trendsalmost 5 years ago
Genetic factors for reproductive aging and vasomotor symptomsNewsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.