- Vol 68 No 05
- Volume 68
- Issue 05
Pruritic rash in vulvovaginal area of 2-year-old girl
Three months ago, a healthy 2-year-old girl presented with a mildly pruritic rash with erythematous plaques, some silvery white, in the vulvovaginal area. She had no vaginal discharge or other symptoms. The rash is now more widespread, and new lesions have recently appeared on her lower back and thighs. What's the diagnosis?
The case
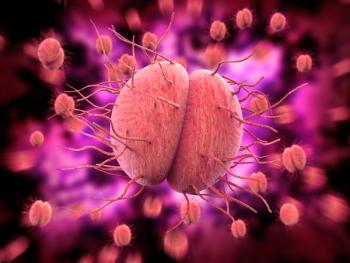
Three months ago, a healthy 2-year-old girl presented with a mildly pruritic rash with erythematous plaques, some silvery white, in the vulvovaginal area. She had no vaginal discharge or other symptoms. The rash is now more widespread, and new lesions have recently appeared on her lower back and thighs (Figure).
Diagnosis
Psoriasis
Discussion
Psoriasis is a common genetic chronic skin condition found in at least 2% of the population.1 Heredity and environmental factors interact to precipitate its development, with a family history observed in 25% to 71% of patients with the disease.2
Environmental triggers include physical injury to the skin, stress, low humidity, and cold weather,and viral/bacterial infections and certain medications can initiate the condition in children.2
All forms of psoriasis (plaque, guttate, erythrodermic, and pustular) observed in adults are likewise encountered in children. The most frequent variant in children is psoriasis plaque (especially localized to the flexural areas) and guttate psoriasis, which may be associated with juvenile psoriatic arthritis.2
In infantile psoriasis, the diaper area is commonly involved (napkin psoriasis) and is usually the first site where plaques are triggered by the Köbner response, owing to constant irritation and maceration. Moreover, in infants, psoriatic plaques often lack scale.2
Vulvar psoriasis is a chronic inflammatory skin disorder that may be isolated or occur in conjunction with psoriasis elsewhere. Vulvar/anogenital psoriasis is one of the most common manifestations of psoriasis in young girls, and a diagnosis can usually be made without a biopsy.3
Differential diagnosis
Vulvar erythema with a rash can be associated with several inflammatory and infectious skin disorders, including psoriasis, atopic dermatitis, contact irritant and allergic dermatitis, lichen planus, lichen simplex chronicus, candida, and tinea. The latter two can be excluded with dermoscopy, potassium hydroxide preparations, and cultures.3
Lichen simplex chronicus is a more severe form of lichenoid dermatitis4, which is seen in atopic individuals and lacks the well-demarcated border of psoriasis.1 In young children with atopic dermatitis, the diaper usually protects the skin from being scratched, and atopic dermatitis does not usually appear in the buttocks or genital area until they are toilet-trained and no longer wearing diapers.
Intermittent symptoms may indicate allergic contact dermatitis,4 which can spread to the entire body, including the scalp, and is accompanied by severe pruritus.2 Allergic contact dermatitis in the vulvovaginal area is common in adult women but rare in children.4
Physical examination and patient medical history are often sufficient to make a diagnosis,3 so it is important to inquire about family history.
Review of our patient’s family history revealed that when her mother was an adolescent she had a similar rash in the genital area that spread to the trunk and proximal extremities and was confirmed as psoriasis on biopsy.
Critical questions to ask in vulvar erythema
Timing. Acute vulvar erythema could indicate an allergic contact dermatitis or candidal vulvovaginitis. Chronic vulvar erythema suggests atopic dermatitis in older children and adults, and seborrheic dermatitis, psoriasis, or lichen simplex chronicus in infants. However, chronic skin diseases can have acute flares. Irritant contact dermatitis may also be chronic if irritating substances are repeatedly used.3
Pruritus. Vulvar atopic dermatitis, allergic contact dermatitis, and candidal vulvovaginitis are generally very pruritic3. Poor hygiene can be another cause of vulvar erythema with pruritus.3
History. The clinician should investigate any previous use of feminine hygiene products that could have led to irritation and erythema and possibly provoked irritant contact dermatitis.
In addition, if used prior to visit, home remedies or medications (and their response or lack thereof) should be reviewed. Also, skin lesions elsewhere on the body and systemic symptoms should be investigated.3
Treatment
Low to mid potency topical corticosteroids are recommended as first-line treatment for genital psoriasis.5 They are typically used twice daily for 1-2 weeks for exacerbations.
Moisturizers and emollients may be helpful in infantile psoriasis and can also be used by older children and adults.5 Once the disorder is under control, nonsteroidal anti-inflammatory creams like calcipotriene, anthralin, tacrolimus, tazarotene, roflumilast (newly approved for 12 and older) and tapinarof (not yet approved in children) may be used.
Systemic therapy is required in a minority of patients with severe, recalcitrant psoriasis1-3 but is not often used for isolated vulvar lesions.3 Systemic agents used to treat widespread psoriasis include retinoids (acitretin), immunosuppressants (methotrexate, cyclosporine, mycophenolate mofetil), and the new biologic agents.3 Treatment should be tailored to patient age and psoriasis type, extent, distribution, and symptoms.2
Environmental changes. Good hygiene and reduced friction are important first-line measures for the treatment of genital psoriasis.1 Patients should be advised to use gentle, nonsoap cleansers in that area and wear loose-fitting clothing to avoid further irritation.5
Vulvar psoriasis can have a significant impact on quality of life and so must be recognized and treated.1 Clinicians should explain that the disease can be managed but not cured.
Our patient
Treatment with low-potency topical steroid triamcinolone 0.025% ointment applied sparingly twice a day for 1 week was initiated and resulted in clearance of rash. The ointment was tapered over the following 2 weeks to as-needed, intermittent use. Topical nonsteroids such as tacrolimus ointment were discussed but not chosen as therapy at this time.
References:
- Kapila S, Bradford J, Fischer G. Vulvar psoriasis in adults and children: a clinical audit of 194 cases and review of the literature. J Low Genit Tract Dis. 2012;16(4):364-71. doi:10.1097/LGT.0b013e31824b9e5e
- Janniger CK, Schwartz RA, Musumeci ML, Tedeschi A, Mirona B, Micali G. Infantile psoriasis. Cutis. 2005;76(3):173-177.
- Trager JD. What’s your diagnosis? Well-demarcated vulvar erythema in two girls. J Pediatr Adolesc Gynecol. 2005;18(1):43-6. doi:10.1016/j.jpag.2004.11.009
- Pichardo-Geisinger R. Atopic and contact dermatitis of the vulva. Obstet Gynecol Clin North Am. 2017;44(3):371-378. doi:10.1016/j.ogc.2017.05.003
- Beck KM, Yang EJ, Sanchez IM, Liao W. Treatment of genital psoriasis: a systematic review. Dermatol Ther (Heidelb). 2018;8(4):509-525. doi:10.1007/s13555-018-0257-y
Articles in this issue
over 2 years ago
Long-acting reversible contraceptive use among adolescentsover 2 years ago
Is this a missed diagnosis of abnormal uterine bleeding?over 2 years ago
Learning to live with changeover 2 years ago
Unplanned military pregnancies are decliningover 2 years ago
Postmenopausal osteoporosisalmost 3 years ago
New molecular test to detect organisms causing vaginitis/vaginosisalmost 3 years ago
Elinzanetant demonstrates rapid reduction in VMS frequencyalmost 3 years ago
Best practices for well woman visits for the adolescent patientalmost 3 years ago
Uterine-sparing techniques for symptomatic adenomyosisalmost 3 years ago
Variety found in quality of data for medications in lactating womenNewsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.