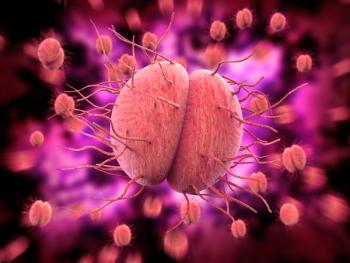
Pathophysiology and Impact of Vulvovaginal Candidiasis
Michael L. Krychman, MD and Jack D. Sobel, MD, talk about the signs and symptoms of vulvovaginal candidiasis as well as its effect on patient quality of life.
Episodes in this series

Michael L. Krychman, MD: Welcome to this Peers & Perspectives® presentation titled, “Expert Perspectives on Recurrent Vulvovaginal Candidiasis Management.” I’m Dr Michael Krychman, a clinical health professor from the University of California, Irvine, located in Orange County, California. It’s a pleasure today to be joined with Dr Jack Sobel from Wayne State University in Detroit, Michigan, to discuss considerations and strategies for the practical management of vulvovaginal candidiasis. Dr Sobel, welcome to our program today and let’s jump right in. I know that you and I both have renewed interest in vulvovaginal candidiasis. The landscape is changing. Before we go into that, let’s talk a little bit about the pathophysiology, the differences between sporadic and RVVC [recurrent vulvovaginal candidiasis]. How do you specifically define that? We want to talk about signs and symptoms, risk factors, and what have you; why don’t you get us started on that?
Jack D. Sobel, MD: Thanks for introducing the subject, Michael. I think to obtain some sort of perspective of what recurrent disease is, we need to recognize that about 70% of women are going to have a vaginal yeast infection sooner or later during their reproductive years. We know that candida vaginitis is just so much less common in postmenopausal women, and it is very rare prior to puberty and onset of menses. Having said that, most women will have an occasional or sporadic attack, and that’s going to be about 80% to 90% of women will have an occasional, or what we call now, a sporadic attack. It may occur with a certain trigger, or it may occur spontaneously without any recognizable triggers. An example of a trigger for that sporadic attack may be recent exposure to an antibiotic given for influenza or for sinusitis, and often for a reason that you really didn’t need to get antibiotics in the first place. Probably half the episodes of sporadic attacks occur without a recognized triggering mechanism. That’s very important because sometimes patients just don’t identify, or physicians are unable to attribute a trigger in sporadic attacks. When we’re talking about recurrent infections, we’ve arbitrarily set this at 3 or more attacks per year, and this is a completely different ballgame. This is a world of repeated attacks, which can be 12 attacks a year. It really creates havoc in the life of a patient because they’re going from one attack to the other. They see practitioners on a regular basis. It has a very profound effect on their normal lives. They’re having symptoms repeatedly or chronically and it has a major impact on their normal, healthy sex lives and seemingly they are taking antifungal agents almost all the time.
Michael L. Krychman, MD: You’re making a good point. Quality of life is certainly a big issue and there’s sexuality issues, relationship issues. You also talked about the medical economic implications of visiting the health care professional quite often. Their symptoms are quite distressing: the burning, itching, pain. Even vulvar and vaginal awareness, where they can’t even sit. For me, in my clinical practice, the impact of VVC and RVVC is astronomical and we have to move away from the concept of “just another yeast infection” as well, right? I appreciate what you’re saying in terms of the impact and, sometimes, lack of risk factors.
Transcript Edited for Clarity
Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.