The Trajectory of Treatment for Recurrent Vulvovaginal Candidiasis
Thought leaders discuss the history of RVVC treatment, including the use of unapproved topical antifungals and the shortcomings of fluconazole.
Episodes in this series

Michael L. Krychman, MD: Let’s talk a little bit about treatment, and what kind of unmet needs or kind of goals there are for RVVC [recurrent vulvovaginal candidiasis]? Where do you think we are? Where do you think we will be? What are some of the problems and pitfalls and shortcomings globally? Talking about the therapeutic need, and then we’ll do a deep dive on some of the newer medications as I know you and I are both very interested in them as well.
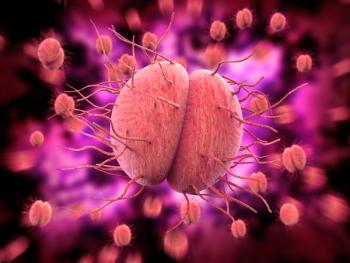
Jack D. Sobel, MD: We get this focus on recurrent candida vaginitis treatment, because acute sporadic—getting a yeast infection once every 10 years, a sporadic episode—is, well over 90% of the time, as you will see, is albicans and whatever you treat it with, topically a local measure or something by mouth, it’s going to get better in a matter of days, just a few days. With recurrent candida vaginitis, the first thing to recognize is the overwhelming majority of the women are going to have recurrent disease caused by the good old regular species, Candida albicans. It may not be 95% anymore, but it’s going to be 85% to 90%. The chances are a woman having repeated infections, you don’t have to run out to do resistance tests and look for do I have a unique unusual species? Eighty-five percent to 90% of recurrences are still going to have the regular old hyphae-producing Candida albicans one. But up to 10% will have nonalbicans species and include even resistant strains of Candida albicans. But it’s 1 of 10. We don’t need to focus immediately on the exceptions. We talk about the 90% that are recurrent due to C. albicans [Candida albicans]. The reason why it’s recurrent is genetic and trigger mechanisms and nothing else. How do we treat it? In the past prior to the onset of some sort of long-term programs, we used to treat recurrent attacks simply by treating each individual attack. You had 10 attacks, you got 10 causes of them. You had 5 attacks per year, you had appropriate therapy for each attack. That was what we were faced in the 1980s and ’90s, just treating each individual attack. But we learned from many other infectious diseases: Can we prevent somebody having 3 or more attacks per year? The answer is yes, but you need a maintenance program. Literally in 1985, with the arrival of the first oral drug called ketoconazole, but no longer available because of toxicity. We learned about the ability to prevent recurrences by using a maintenance program. The antifungal mechanisms that we’ve used are based on using an induction dose, which takes a symptomatic patient who’s got acute flare of a recurrent disease today, she takes an induction dose, most commonly in the last 30 years it’s been fluconazole. She ends up within a week or 10 days she’s asymptomatic. This usually requires more than 1 tablet of fluconazole. Then you place her on a maintenance program, and the maintenance program continues for approximately a minimum of 6 months. During the minimum you give them a maintenance dose. That was the biggest advance firstly, with ketoconazole and then itraconazole, and it’s been fluconazole that has been the dominant treatment mechanism for recurrent candida vaginitis just for the last 20 years.
Michael L. Krychman, MD: Yeah, your point is well taken about the utilization. But again, you’re saying that’s what we’ve been doing, but it’s certainly not FDA [Food and Drug Administration] approved. There are also some shortcomings with fluconazole. I certainly have seen changes in liver functions, alcohol may affect the liver, fluconazole, as well. There are some monitoring issues that may be of concern. And again, if you see what’s going on in the community, we certainly see people using boric acid, probiotics, limited data, etc.
Transcript Edited for Clarity
Newsletter
Get the latest clinical updates, case studies, and expert commentary in obstetric and gynecologic care. Sign up now to stay informed.